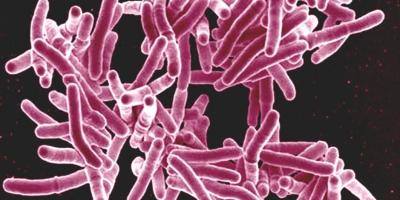
Tuberculosis or TB, one of the top infectious diseases responsible for mortality worldwide, is one of those diseases that majorly affects those in the lower socio-economic group.
The 2023 UN General Assembly High-Level Meeting on TB reinforced the 2018 commitments and targets, setting out new targets for the period of 2023-2027. The new targets include reaching 90% of people in need with TB prevention and care services and using a WHO-recommended rapid test as the first method of diagnosing TB.
The meeting also highlighted the provision of health and social benefit packages for all people with TB and the securing of at least one new TB vaccine that is safe and effective. The meeting also recommended closing funding gaps for TB programme implementation and research by 2027.
While we talk about funding at a macro level, TB continues to inflict financial hardships on millions of Indians every year. India has the highest TB burden across the world contributing to about 27% of all the TB cases, according to the WHO’s Global TB report 2023.
While India’s National Tuberculosis Elimination Programme (NTEP) covers diagnostic and therapeutic costs of TB treatment, many seek TB care privately for a vast variety of reasons with the most prominent among them being stigma.
People living with TB experience financial distress due to both direct and indirect costs. Taking loans, borrowing money, selling land, gold jewellery or any other assets are some measures people take to cover the cost of care.
The picture I paint is not a one-off scenario. ‘Catastrophic’ spendings necessitated by TB, as highlighted by WHO, are direct and indirect costs of TB diagnosis and care which amount to over 20% of the TB patient’s household’s annual income.
Of the 30 high TB burden countries, estimates of the percentage of the population facing catastrophic health expenditures are particularly high for India along with Angola, Bangladesh, China, Nigeria, Sierra Leone and Uganda, the global report says.
The direct cost includes medical costs (involving registration, consultation, hospitalisation, investigation, or medication) and non-medical costs (food, travel, and nutritional supplements). Indirect costs comprise an overall loss of wages due to productivity loss, missed work, loss of time, loss of income, and caregiving work.
It is more alarming as direct costs of care from private physicians are manifold compared to that incurred by individuals who are treated by NTEP (National TB Elimination Programme) providers under the government’s set-up.
The high costs associated with TB entrap the affected population into a vicious cycle of poverty and disease which is far from WHO’s ‘End TB’ goal, including the target that no TB patients and their households should face catastrophic costs due to the disease.
As per the WHO Global TB Report 2023, about half of the TB patients and their households suffer catastrophic (>20% of annual household income) total costs. A report from WHO and Treatment Action Group (TAG) shows us that there was a decline in global funding for essential TB services, from US $ 6.5 billion in 2019 to US $ 5.8 billion in 2022 which is less than half of the global target of US $ 13 billion.
Current health expenditure (% of GDP) in South Asia in 2020 was less than 4.18 and significantly lower in countries like India, according to World Bank data. According to The Wire‘s news report, in the interim Indian budget presented for the year 2024-25, the budget allocation for the department of health and family welfare, the department of health research and key nutrition programmes have dipped for the fiscal year 2024-25 as compared to 2023-24 budget estimates, when adjusted for inflation.
Contrary to the allocation of Rs 86,175 crores (as per budget estimates) for the department of health and family welfare in FY 2023-24, the allocation for 2024-25 increased to Rs 87,656 crores. However, when considering inflation at a rate of 5%, this apparent increase actually amounts to a decrease of 3.17% in real terms, the news report says. Thus, the budget for the health and family welfare department has actually decreased when adjusted for inflation.
The goal to achieve elimination of TB can be completed by reaching the lower socio-economic and remote sections of vulnerable communities. Inadequate funding and inaccessible resources are major hindrances in reaching the desired goal of ending TB worldwide.
The global aspirations to eliminate TB by 2030 reflect crucial ambition and determination. India aims to eliminate TB by 2025. However, with current funding levels and opportunities, the aim to end the TB crisis by 2030 appears challenging to achieve unless addressed timely, leaving vulnerable communities at risk of further devastation due to TB in the latter half of the 21st century.
Encouragingly, ongoing scientific advances such as newer tools to screen and diagnose TB and newer treatment regimens, as well as new vaccines in the pipeline offer genuine promise in combating the epidemic by 2030. Yet, achieving this goal will demand a significant increase in funding and finding innovative ways to reduce direct and indirect costs of TB care to disrupt this vicious circle.
Increasing awareness of the government’s services for TB elimination, continued decentralization of services and dispelling negative attitudes about the national TB programme may encourage impoverished affected people to avail free care.
Social determinants of health, such as poverty, malnutrition, and crowded living conditions are equally important factors which are overlooked while planning a comprehensive TB control strategy in many South Asian countries, including India.
Farhat Mantoo joined Doctors Without Borders/Médecins Sans Frontières (MSF) in 2003 and has been working in different capacities nationally as well as internationally. Currently, she is the Executive Director of MSF South Asia. She has a specialisation in medical anthropology, communication, hospital management and human resources apart from being trained in humanitarian assistance linked to international humanitarian affairs.





